Mesothelioma Pathology Outlines
Mesothelioma Pathology Outlines
The histological appearance ranges from pure epithelial to the pure mesenchyme forms.
A combination of above patterns may be present. It is important for the pathologist to be aware of these patterns to make a histologic differentiation between DMM and other neoplasms.
Defination / General
Malignant mesothelioma arises from mesothelial lining of pleura, peritoneum, pericardium and tunica vaginalis - pleural mesothelioma is the most common of these.
Etiology
Smoking is not a risk factor
Risk factors include:
- Asbestos exposure:
- Usually a prolonged latency period
- Studies do not show a linear dose / response relationship between asbestos exposure and malignant mesothelioma
- The role of amphibole (crocidolite) asbestos is well established
- Crocidolite is a much more potent carcinogen than chrysotile (serpentine form); it accounts for 95% of asbestos used, and so is the main cause of malignant mesothelioma
- Radiation
- Erionite: very carcinogenic mineral fiber used in gravel roads
- SV40 virus (association is not clear)
Diagnosis
- Current standard requires biopsy followed by immunohistochemistry using a large panel of markers to distinguish from other tumors
- If available, or immunohistochemistry results are not clear, EM studies should be conducted
Laboratory
- Soluble mesothelin-related peptide (SMRP) levels may correlate with disease status
Radiology description
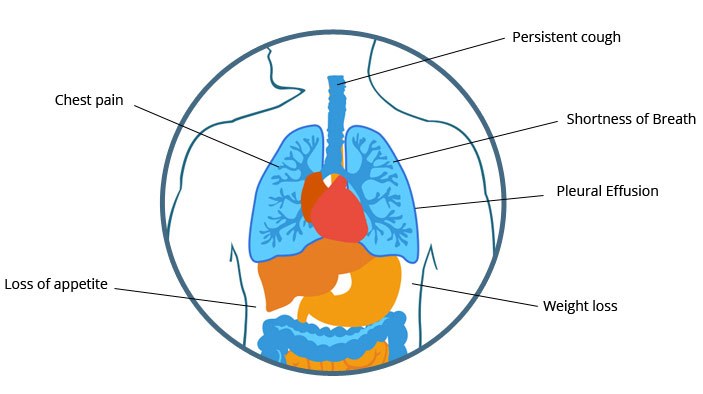
- Strongly suggestive of malignancy: pleural effusion, pleural wall thickening, circumferential pleural thickening involving the mediastinal pleura, nodular pleural thickening
Prognostic factors
Epithelioid histology is favorable
Sarcomatoid histology and mixed tumors are unfavorable
Treatment
Stage I - III cases: induction chemotherapy with pemetrexed and cisplatin or surgical exploration
Surgical treatments include pleurectomy / decortication or extrapleural pneumonectomy (EPP)
Talc pleurodesis or pleural catheter, for management of pleural effusions
Both chemotherapy and radiotherapy improve long term survival
Electron microscopy description
Long, slender microvilli (length > 15× diameter) with tonofilaments but without glycocalyx
No lamellar bodies (adenocarcinoma has short stubby microvilli)
Most useful in epithelioid variant and moderately well differentiated tumors
Sarcomatoid mesotheliomas do not show mesothelial features by EM
Limitations:
- Ultrastructural features of adenocarcinoma and mesothelioma overlap
- EM may not be helpful in poorly differentiated tumors
Clinical features
Progressive shortness of breath
Chest pain, possibly unilateral
Cough, fever, malaise, myalgia and weight loss.
The three broad histological types:
(i) Epithelial ; (ii) Sarcomatas / Fibrous ; and (iii) Biphasic or mixed.
50% - Pleural and 75% - Peritoneal mesothelioma.
30% are biphasic.
15% - 20%- Pure sarcomatas subtype.
Recognition of histopathology patterns of diffuse malignant mesothelioma in differential diagnosis of pleural biopsies.
Epithelial Mesothelioma:
In diffuse mesothelioma epithelial DMM are the most commonly diagnosed histologic type.
Tubulopapillary Pattern:
Mixture of small tubules and papillary structures with fibro vascular cores, often with clefts and trabecular.
In well differentiated tumors the fibro hyaline papillae are lined by neoplastic mesothelium cells - (uniformly cuboidal cells with large vesicular nuclei and prominent nucleoli).
Psammoma bodies may be present.
Differential diagnosis: Adenocarcinoma metastatic to the pleura.
Acinar Pattern:
Characterized by acinar or gland like structures.
Differential diagnosis: Metastatic adenocarcinoma.
Adenomatoid Pattern (also termed micro glandular):
Small gland-like structures lined by bland flat to cuboidal c
ells.
Differential diagnosis: Metastatic adenocarcinoma.
Small cell pattern:
Sheets of monotonous small hyper chromatic uniform cells with a high nucleocytoplasmic ratio.
Differential diagnosis: This variant may mimic small cell carcinoma or lymphoma.
Nuclear karyorrhexis and haematoxyphilic vessels are not a feature in mesothelioma.
Lymphoma is distinguished from small cell variant of mesothelioma by immunohistochemical examination.
Deciduous Pattern:
Identified in the pleura of elderly patients.
Histologically the tumor is characterized by proliferation of large, round to polygonal cells with sharp cell borders, abundant glassy eosinophilic cytoplasm, and round vesicular nuclei with prominent nucleoli.
Differential diagnosis: Squamous Cell Carcinoma, trophoblastic neoplastic, gastrointestinal autonomic nerve tumor, anaplastic large cell lymphoma, oxyphilic variant of ovarian clear cell carcinoma.
Signet Ring (Lipid-Rich) Pattern:
Tumor cells exhibiting secretory change with cytoplasmic vacuolation.
Differential diagnosis: Metastatic Signet ring cell adenocarcinoma.
Clear Cell Pattern:
There are tumor cells with clear cytoplasm. Other patterns may be present in the tumor.
Differential diagnosis : Clear cell tumor that are metastatic to the pleura.
Example: Renal cell carcinoma, clear cell carcinomas of the lung, clear cell melanoma.
Adenoid Cystic:
Cribriform and tubular growth patterns set in a fibrous stromal.
Differential diagnosis: Metastatic adenoid cystic carcinoma and adenocarcinoma.
Solid Pattern: Well differentiated and poorly differentiated:
Well differentiated- Nests and sheets of round cells with abundant cytoplasm and round, vesicular nuclei with prominent nucleoli. Mitoses are usually not prominent.
Differential diagnosis: Benign reactive mesothelium hyperplasia.
Poorly differentiated- Monotonous sheets of cytological malignant polygonal cells with abundant glassy eosinophilia cytoplasm with uniform nuclei.
Differential Diagnosis: Lymphoma and large cell carcinoma.
Sarcomatous Mesothelioma:
Sarcomatoid mesothelioma is composed of a fascicular proliferation of spindle cells with oval nuclei, scanty cytoplasm and occasionally prominent nucleoli.
Tumor cells display a fibro sarcoma-like appearance with elongated fascicles showing herringbone formations and abundant intercellular collagen deposition.
Tumor may show a prominent storiform appearance indistinguishable from that of malignant fibrous histiocytoma.
Sarcomatoid mesothelioma show i) more atypical ii) display mitotic activity iii) foci of necrosis.
Lymphohistiocytoid Mesothelioma:
Histologically, the tumour is characterized by a diffuse discohesive proliferation of atypical histiocytoid cells intermixed with a marked lymphocytic and moderate plasmacytic infiltrate.
In lymphohistiocytoid mesothelioma, the demonstration of cytokeratin expression by the neoplastic cells is the most useful diagnostic finding that allows exclusion of other neoplasms with which this entity may be confused.
Desmoplastic Mesothelioma:
This is a rare variant of malignant mesothelioma with a storiform collagen pattern, collagen necrosis, bland a cellular collagen and focal cytological features of malignancy.
Though rare, it is important to recognize this variant and distinguish it from a pleural plaque, nonspecific reactive pleural fibrosis, pleurisy, rheumatoid disease, or, rarely, spindle cell sarcomas.
Biphasic (Mixed) Mesothelioma:
Characterized by a combination of epithelial and sarcomatoid patterns.
Differential diagnosis: Carcinosarcomas, biphasic pulmonary blastoma, and biphasic synovial sarcoma.
Miscellaneous Pattern:
Pleomorphic: Both epithelial and sarcomatas pattern are present; there are tumor giant cells and anaplastic cells.
Transitional: Tumor cells with a “transitional” appearance, displaying both epithelial and sarcomatas features in the same cell.

.png)